Filling the Physician Shortage on Maryland’s Eastern Shore
With a commitment to addressing rural health disparities and the challenges faced by Maryland’s rural Eastern Shore residents, the University of Maryland School of Medicine (UMSOM) has launched the Rural Health Equity and Access Longitudinal Elective (R-HEALE). The program is designed to train and place incoming medical students in Eastern Shore health care practices. It has received $1.4 million in state funding to launch the effort with added funds provided by the University of Maryland, Baltimore (UMB); the University of Maryland Eastern Shore (UMES); the Rural Maryland Council; and philanthropic donors.
The program, in partnership with UMES, has accepted six current first-year medical students with an interest in rural health. Three students have been awarded full-tuition scholarships with a commitment to working on the Eastern Shore for four years after completing residency training. The students will have didactic and mentoring sessions in Baltimore followed by research and clinical experiences on the Eastern Shore. The long-term goal is to ultimately support 10 new students interested in rural health in this elective program each year, with 10 full in-state tuition scholarships.
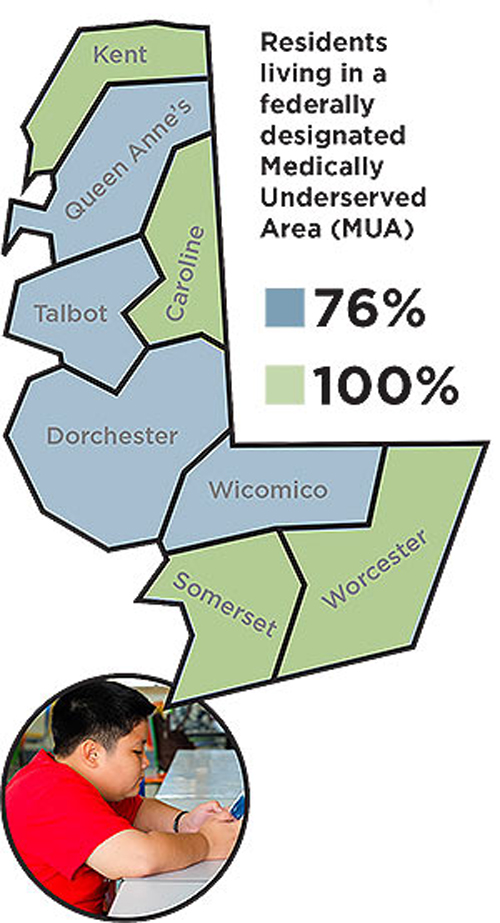
Nearly the entire Eastern Shore is designated by the federal government as a medically underserved area and as a “health professional shortage area,” which means residents often lack access to the medical care they need to address pressing health concerns. The five counties in Maryland with the fewest primary care physicians per capita are all in the Eastern Shore region, with Caroline County having only one health provider per 2,500 state residents compared to Baltimore County, which has one provider per 1,000 state residents.
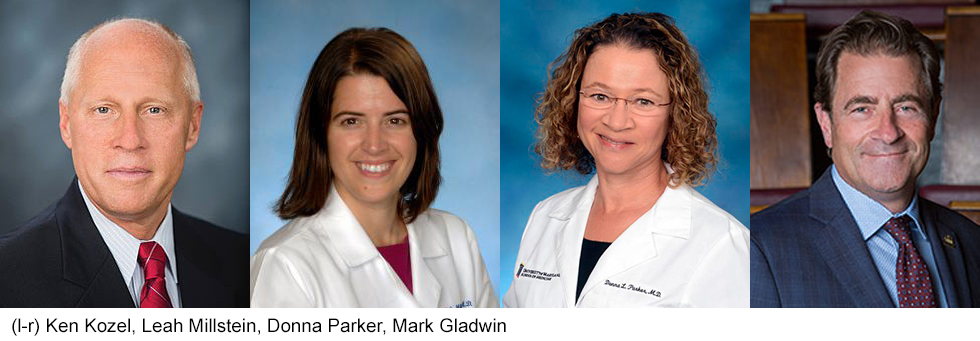
“People living in rural areas on the Eastern Shore often face challenges with access to medical care, which may lead them to skip important appointments or travel an hour or more to Annapolis or Baltimore for the treatment they need,” said Donna Parker, MD, professor and senior associate dean for undergraduate medical education, UMSOM. “With this program, our goal is to develop a cohort of up to 10 additional physicians annually to address the health care shortage. By increasing access and reducing long provider wait times, we hope to improve health outcomes in the region.”
According to a recent study conducted by UMSOM researchers, residents of rural areas face significantly higher risks of developing complications from chronic diseases such as diabetes. Their findings revealed that those living in small towns, with fewer than 2,000 people, were 10 percent more likely to have a heart attack, 5 percent more likely to experience heart failure, and 4 percent more likely to have end-stage kidney disease than those living in large cities.
“More than 1 million Maryland residents live in underserved areas and the largest proportion come from rural Eastern Shore counties. This is associated with higher infant mortality rates, shorter life expectancy, and poor health outcomes including complications from diabetes and high blood pressure,” said Mark T. Gladwin, MD, the John Z. and Akiko K. Bowers Distinguished Professor and dean, UMSOM, and vice president for medical affairs, UMB. “We want to provide patients with access to the long-term care they need to both prevent and effectively manage chronic diseases. This first class of physicians represent our long-term commitment to improving rural health outcomes and creating a better quality of life for Marylanders on the Eastern Shore.”
The R-HEALE program aims to include a program held on the UMES campus where students will be introduced to foundational courses on the social determinants of health and barriers to care access in the region. Lecture topics likely will include health disparities, social justice and rural medicine, and patient care. Students will be paired with a physician mentor on the Eastern Shore, allowing them to observe patient interactions in a rural health care setting throughout their years in medical school.
“I am very excited to receive mentorship from doctors who are serving in rural health,” said Tahreem Riaz, an R-HEALE scholarship student who is from a rural area in Punjab, Pakistan. “I think it’s a great opportunity to learn and will provide us with the ability to face the challenges of rural practice while finding solutions to complex issues.”
In the summer of their first year, the students will engage in a rural health-based research project. They also will have opportunities to work clinically on the Eastern Shore during their third and fourth years to complete clerkships and electives.
“This is a truly longitudinal experience, where students will engage in collaborative learning throughout the four years of medical school, so they can graduate with the range of skills necessary to serve the needs of the patient population on the Shore,” said Leah Millstein, MD, course director for the R-HEALE Program and associate professor of medicine, UMSOM.
“I hope to use my knowledge of the community to better connect with patients and form trusting relationships that will empower them as they navigate the health care system,” said Sarah MacDonald, and R-HEALE scholarship student who grew up in Salisbury, Md.
The R-HEALE program is partnered with UMES, University of Maryland Shore Regional Health (UM SRH), TidalHealth, the Dorchester County Health Department, the Eastern Shore Area Health Education Center, and the Maryland Area Health Education Center. Additional partnerships with Eastern Shore health care organizations are to be established to place students in various clinical experiences during their training.
“Strengthening our provider workforce is a top priority at UM SRH, and programs like R-HEALE will help us attract providers who want to practice in rural communities,” said Ken Kozel, MBA, FACHE, president and CEO of UM SRH. “We greatly appreciate our partnership with the School of Medicine toward enhancing access across the Shore.”
Learn more about R-HEALE.



